There’s an alternative to the traditional fee-for-service healthcare model. Ryan Vasilik, CFA, Equity Analyst, sheds light on the opportunities that abound with value-based care.
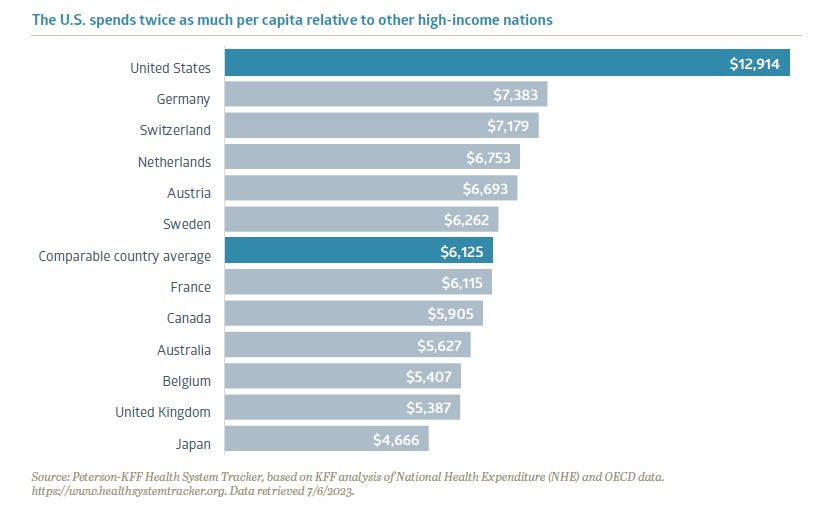
For decades, narratives about the escalating costs of healthcare and its impact on affordability have remained at the forefront of American concerns. Most people either know of, or have personally experienced, financial hardship when dealing with medical issues. In fact, medical bills are the leading cause of personal bankruptcy in the U.S.1 Compared to other industrialized nations, the U.S. spends twice as much per capita on healthcare services. High healthcare spending by itself isn’t necessarily a negative; shockingly though, despite spending twice as much as its peers, the U.S. also ranks dead last on measures like life expectancy and patient satisfaction.
While there are many stakeholders involved in our healthcare system, there is no single villain responsible for driving up costs and there is no silver bullet solution. Fortunately, new healthcare delivery alternatives are emerging to help bend the cost curve and substantially improve patient outcomes. One new healthcare paradigm to address these challenges is value-based care. We believe the emergence of value-based care will revolutionize our perception of the U.S. healthcare system and holds the potential to enhance cost efficiency, patient outcomes, and open new horizons for entrepreneurs and established companies alike.
A Game-Changing Approach
Value-based care (VBC) is a transformative approach to delivering healthcare, where stakeholders compete on the quality of patient outcomes instead of quantity. All parties have skin in the game and are financially at risk if patient results deteriorate. VBC healthcare providers receive a risk-adjusted annual fee per patient from insurance payors and are responsible if patient complications arise. Healthcare providers and payors are aligned to properly diagnose, direct, and treat patients throughout the medical episode, thus focusing on preventative care and keeping patients out of the hospital.
Under this new model, healthy patients and provider profitability go hand-in-hand. The goal for the provider is to generate excess profit by managing patient pools in a more efficient manner. Traditionally, the U.S. healthcare system has employed a “fee for service” delivery model, where providers are paid on patient visits. This model has been criticized due to the potential for conflicts of interest where the provider benefits the more a patient utilizes medical care. Insurance companies complicate the issue, as they are often responsible for covering the medical bills of patients and may attempt to ration care or shift costs to protect their bottom line. Value-based care is a new form of competition that focuses on long-term medical outcomes for patients and lowers costs for payors in a sustainable way. The beauty is that it corrects the downfalls of the fee-for-service model. While fee-for-service treatment is frequently criticized for waiting for a patient to get sick before receiving care, value-based medicine relies on investing in systems to help providers diagnose or even prevent illnesses early and match patients to the appropriate care facilities to improve their lives throughout the healthcare continuum.
 The push for value-based care originated through Medicare Advantage, an additional insurance program for seniors that offers supplementary benefits alongside regular Medicare. Utilizing a VBC model within the Medicare Advantage population was a logical first step, due to the significant potential for reducing costs in this program. Although comprising only one-sixth of the U.S. population, individuals aged 65 and above account for over one-third of all medical expenditures. The VBC model has been widely viewed as a success within Medicare Advantage. Today, roughly six million Medicare Advantage patients have physicians who contract with VBC providers.2 This figure is projected to increase as Medicare officials have expressed a goal to establish value-based care relationships for every Medicare beneficiary by 2030.3
The push for value-based care originated through Medicare Advantage, an additional insurance program for seniors that offers supplementary benefits alongside regular Medicare. Utilizing a VBC model within the Medicare Advantage population was a logical first step, due to the significant potential for reducing costs in this program. Although comprising only one-sixth of the U.S. population, individuals aged 65 and above account for over one-third of all medical expenditures. The VBC model has been widely viewed as a success within Medicare Advantage. Today, roughly six million Medicare Advantage patients have physicians who contract with VBC providers.2 This figure is projected to increase as Medicare officials have expressed a goal to establish value-based care relationships for every Medicare beneficiary by 2030.3
Beginning with the PCP
The foundation of value-based care begins with the primary care physician (PCP). Providing concierge-level care, primary care physicians and their team interact with patients up to ten times per year at no additional cost to patients. Doctors spend a greater amount of time with their patients to monitor their health and provide follow-up care to make sure patients are achieving their health goals. These additional interactions are not trivial; for example, doctors found that weighing patients who have congestive heart failure once a day can help identify whether a patient’s heart failure is deteriorating. This additional data can help the patient’s medical team intervene earlier, potentially halt the deterioration, and keep the patient out of the emergency room.
Unfortunately, data has shown that under the current system, many patients use the emergency room as their primary care doctor, racking up thousands in unnecessary medical bills and often leading to an expensive downward spiral. Some of the lowest hanging fruit for cost reduction is directing patients to the appropriate center as an alternative to expensive emergency room visits. Steering patients to lower-cost locations, such as suburban offices instead of city centers or even coming to the patient’s own home, can achieve the same or potentially superior medical benefit at a fraction of the cost. Ultimately, under VBC, a healthier patient leads to less medical spending that needs to be reimbursed by payors, leading to better healthcare outcomes at lower costs.
Nearing an Inflection Point
The value-based care industry has experienced enormous growth over the past few years, and we are now reaching an inflection point. As the healthcare industry gets more comfortable with VBC models, we believe the next evolution will be focused on three key areas: optimizing care coordination, broadening data capture, and expanding VBC to reach new patient populations.
The move towards VBC within specialty chronic conditions, like kidney disease or diabetes, is a logical next step. Managing chronic diseases involves interacting among multiple specialty physicians and teams. By organizing care coordination specifically around these diseases, we can break down information barriers and eliminate redundant treatments.
Payors will increasingly demand clinical studies from drug and medical device companies that not only demonstrate the efficacy of the product, but also quantify the total lifetime savings generated by these products. Companies that present data showing how their drugs or devices both directly and indirectly prevent future complications will earn higher status in formularies.
The principles of value-based care can also be applied to younger patient demographics. Helping facilitate this demographic expansion are private healthcare information technology companies who provide software and patient management insights that enable providers to enter into value-based relationships at minimal financial risk. As healthcare providers and payors accumulate more data, they can adopt best practices and realize the benefits observed in senior populations.
Change is Not Impossible
As a nation, we all have a stake in healthcare reform and improving patient care. The destiny of the U.S. healthcare system is not predetermined, and it would be a mistake to assume that change is insurmountable. Each year, a new class of visionaries sets out to tackle the healthcare cost dilemma.
While still in early days, we believe value-based care can materially shift the U.S. healthcare delivery model. Given the nascent state and dynamic evolution of the model, it presents a golden opportunity for entrepreneurs and investors, promising lucrative rewards for those who emerge as winners. Monumental progress has been made since the beginning days, and we have real world data measured over years that shows VBC works. The shift towards this new model will not happen overnight, but the evidence is clear that our path forward to reimagining healthcare is through value-based care.
1 Bedayn, J. (2023, April 17). States confront medical debt that’s bankrupting millions. AP News. https://apnews.com/article/medical-debt-legislation-2a4f2fab7e2c58a68ac4541b8309c7aa.
2 U.S. Centers for Medicare & Medicaid Services. (2023, April 5). Medicare Advantage Value-Based Insurance Design Model Extension Fact Sheet: CMS Innovation Center. Innovation Center. https://innovation.cms.gov/vbid-extension-fs.
3 King, R. (2022, April 29). CMMI’s Liz Fowler calls for better approach to educating public, lawmakers on value-based care. Fierce Healthcare. https://www.fiercehealthcare.com/providers/cmmis-liz-fowler-calls-better-approach-educating-public-lawmakers-value-based-care.
Recent Insights
Bailard Appoints Dave Harrison Smith, CFA, as Chief Investment Officer
Bailard is pleased to announce that, as of today, Dave Harrison Smith, CFA, has been promoted to Chief Investment Officer. He succeeds Eric Leve, CFA, who held the role for more than a decade and will continue with the firm as a portfolio manager, fully focused on international markets.
July 1, 2025
Country Indices Flash Report – June 2025
Tariff negotiations intensified as the July 9th reciprocal tariff deadline nears, though the Trump administration signaled flexibility on the cutoff for countries negotiating in “good faith.” The U.S. and China secured a high-level framework that included a key rare earths deal and a tariff truce extension to August 11th. Meanwhile, the UK finalized a 10% tariff rate after a threatened 27.5%; talks are swiftly progressing with the EU.
June 30, 2025
Mike Faust Awarded 2025 Advisors to Watch by AdvisorHub
Michael Faust, CFA, ranked in the top five of AdvisorHub’s Advisors to Watch for the second year—recognizing his standout leadership at Bailard.
June 24, 2025
Keep Informed
Get the latest News & Insights from the Bailard team delivered to your inbox.